Why is your OB so tired?
Jul 12, 2024
I wrote this post a few months ago while sitting in a call room at 6pm. I’ve been hesitant to post it because it seems angry. Truthfully, I was probably angry when I wrote it. I’ve been working on consciously choosing thoughts that serve me, and I’m not as angry most of the time as I was then. Writing helps that.
But this post is real and it’s human and so is every obstetrician out there. Human. And again, my goal for this blog is to present my life in medicine as it is – the good, with the bad. So here it is.
I’m on call on the weekends for 3 days. I came in at midnight on a Saturday night after working all day Friday. I was still there the next night at 6PM because I had a patient who desired a VBAC and I was trying to give her every opportunity to achieve that goal, even though she came in with ruptured membranes at fingertip (½ cm) dilated and 10 hours later was 1 cm dilated.
I’d like to outline some challenges faced by today’s obstetrician. These issues are contributing to early retirement of OBGYNs and will likely exacerbate the access to care issues that are already occurring in rural areas and are projected to occur in the coming years. These are the reasons that experienced obstetricians are leaving their practices for laborist jobs or giving up providing OB care altogether.
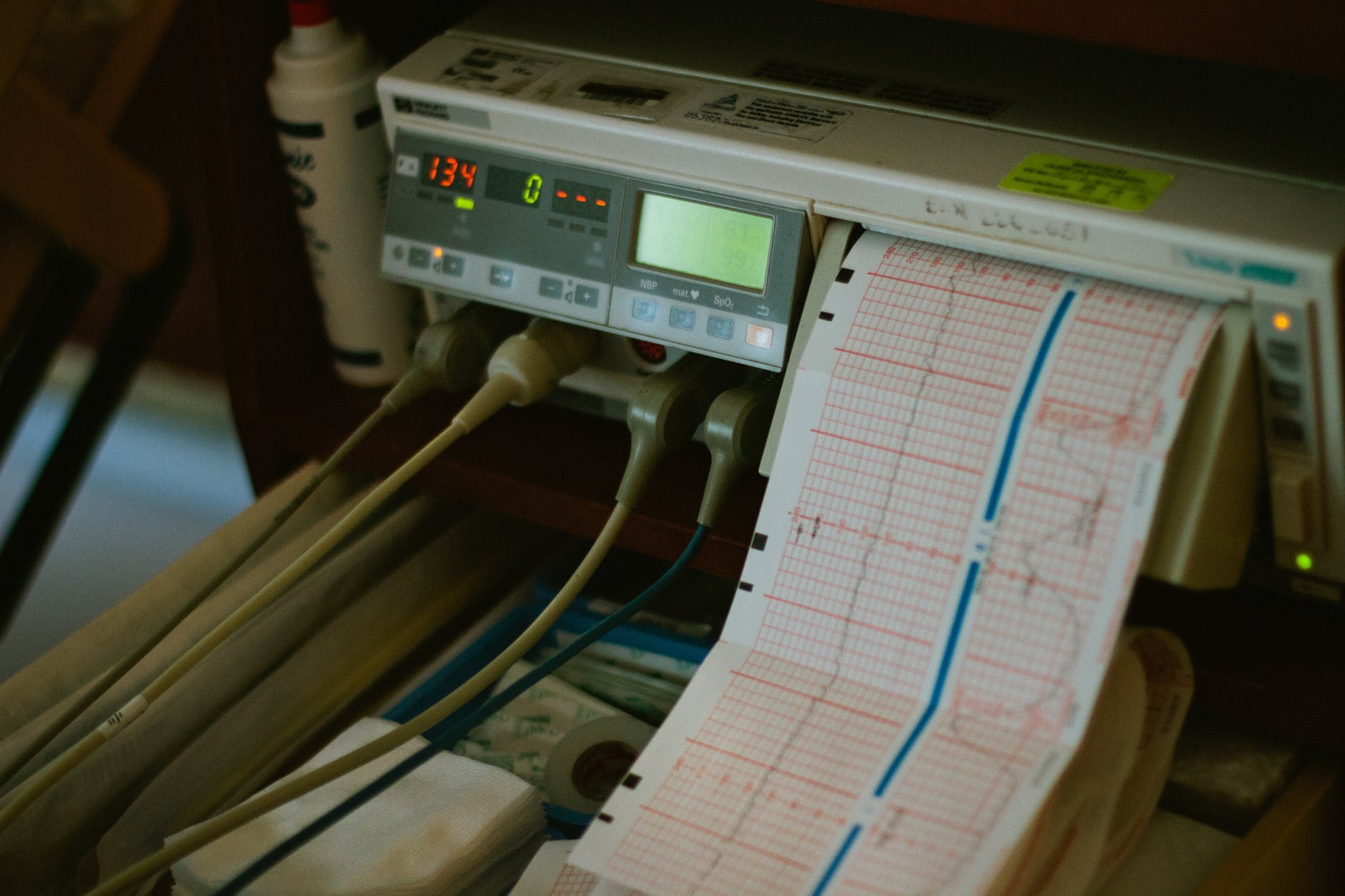
1. OB is exhausting. It’s been described as “hours of boredom punctuated by moments of terror.” We sit around on call for hours only to be called for an uneventful delivery in the best-case scenario (we all still think every delivery is magical too, but 10-15 magical deliveries a month become magically uneventful after a while). In the worst case scenario we get the “baby’s down, we need you now” call and run down the hall from a dead sleep, enter the room to the too-slow heartbeat with mom on all fours, oxygen mask running, people gathering to help, techs waiting to hear if they need to open the OR, and have to make the call to do a section or wait for the heart rate to climb back up.
2. I’m tired from packed office days, with more and more added on patients. Our patients need to see us, and our days are already full, but nobody else sees pregnant women. So we add more on. We operate on GYN patients and go back to packed office schedules where we’re already running behind from the minute we open the door because we need the volume to pay the overhead as the costs of running a practice increase and reimbursement from insurance companies is stagnant or decreases.

3. We don’t value women’s health enough in this country to pay for GYN procedures anywhere near the rate we pay for urologic procedures on men’s genitalia. There is a slide from a conference circulating on social media about RVUs (relative value units, which determine how docs get paid for the care they provide) for similar GYN and urology procedures (biopsy of the skin of the vulva or vagina vs biopsy of the penis or scrotum, for example). Across the board, the women’s health procedures (which, not coincidentally, are largely also performed by female gynecologic physicians) are reimbursed lower than comparable procedures performed on men, by mostly male physicians. Not to mention the incredible bargain that is maternity care in this country – a bundled payment for the entire 10-month pregnancy and postpartum course and delivery itself, that reimburses us less than the anesthesiologist who does your 15-minute epidural. This disparity in pay, that I can’t help but believe is gender related because we are primarily women taking care of women, is exhausting.
4. Online reviews (to which we cannot respond because of federal privacy laws) are exhausting. We deal with and try to smooth over situations outside our control. We deal with irate patients who’ve been waiting for their birth control refill visit while another woman next door is miscarrying. If only I could tell her why I’m running late when she yells at me for her wait time, maybe she’d see that it’s sometimes good to be the one who’s waiting in the doctors office, rather than the one who has to be seen urgently.
5. I’m also frustrated by having to convince people to allow me to use my knowledge and experience to care for them. I’m sorry that you don’t like the standard of care medical advice that I give you. I’m really trying to get the best outcome I can for you when I recommend induction due to new onset hypertension in pregnancy at 39 weeks. I’m recommending glucose tolerance tests to screen for gestational diabetes because I care if your baby gets macrosomic and can’t maintain their sugars after delivery. I care if you have a severe laceration while you’re delivering and have fecal incontinence afterward, or have a shoulder dystocia and your baby has arm paralysis after delivery. I’m not trying to ruin your birth plan. I’m trying to save your life and health and that of your baby. Please do not then go blast me on social media when you don’t like the advice I give, or when the unpredictable process of birth doesn’t follow your detailed plan for the process. I’m all about helping to achieve your preferences if those preferences remain medically advisable in your situation, but birth can’t be planned.

6. I’m tired due to ever increasing mandates by hospitals and insurance companies of what boxes I have to click in a computer program that runs slower than old 90s AOL dialup while I see these ever increasing numbers of patients. These programs are so locked down and have so many levels of security that it takes 10 min to get logged in, and I spend half my day staring at an hourglass waiting to move between screens. I have an EMR in my office and whole different one at the hospital. They don’t play well together. It takes forever to get logged into the hospital EMR from my office or home (if I’m ever even successful – sometimes it just doesn’t work). Yet I’m expected to enter my H&P directly. Enter my orders directly. Click all the right boxes to achieve the hospital’s quality metrics. Click all the right things to order labs from the office on patients, chart the right numbers of HPI elements, ROS elements, exam elements, medical decision making points, and make sure all the history is entered correctly.
7. I’m tired from worrying constantly about getting sued. We expect perfection in this country as far as health outcomes, especially when it comes to delivering babies. We can’t have perfection. Yes, labor is a natural process, but nature is a horrible obstetrician. Labor still carries risk of death for mom and baby, even if we do everything perfectly. All throughout history, women have died in childbirth, or their babies have died at delivery, or both. Walk through a turn of the century cemetery and see all the baby graves, and the graves of young women. A little over 100 years ago, modern obstetrics began to make birth much, much safer than it was when women delivered in homes with the help of trusted friends or family members. We’ve now made it so safe that we’re victims of our success, because people now expect that nothing bad will ever happen to a mom or baby in labor, and if it does, they sign up to play the medical lottery. “You may be entitled to compensation” is part of the reason for my exhaustion. Worrying about being sued with every decision I make is exhausting.

8. I’m tired from reading article after article about how OBs suck. Really, NPR and many other news outlets seem to be on a mission to point out all the ways obstetricians are awful human beings out to harm women by doing c-sections so we can make it home in time for dinner. Homebirths are not the solution to the maternal health crisis despite what you read on Facebook. Women die in this country for LACK of access to high tech care during pregnancy and between pregnancies, not BECAUSE of high tech care. CNMs, midwives trained to international midwifery standards, are an important part of the team caring for women, and that role cold be expanded by improving the tort reform situation in this country so that obstetricians can feel more free to integrate them into our systems of care and not get sued for someone else’s decision making. Lay midwives or CPMs, on the other hand, are high school graduates who watched a few deliveries after a home study course. They don’t disclose this dearth of training. Poorly trained homebirth midwives don’t disclose that they don’t carry malpractice insurance, don’t have a collaborative relationship with a physician in case you need one to help you have your baby if your beautiful home birth turns into a need to have more medical intervention. Are there some bad apple OBs out there? Absolutely. Just like in every other field of medicine and just like in any other industry. The good ones among us are trying to root them out because they give all of us a bad name. Can we improve? Absolutely. And we’re taking steps to actively try to improve. Look at AIM, FPQC, CMQCC. We’re trying to improve care for women in this country because it is our passion. Why else would I be here all day on a Saturday waiting for one woman to deliver the way she wants to deliver? We’re working on it. Please stop painting OBs as the bad guy in the story, because this is not making care for mothers safer. These stories drive a wedge between us and our patients. They disrupt the doctor patient relationship. They make patients mistrust our motives when most of us really just want to give the best care we can give our patients and have happy moms and babies leave the hospital together. If we were in it for money or lifestyle, we picked the wrong field.
Coaching has helped me personally, so I trained to become a coach so that I can share the same tools with you.
Book a free introductory session now.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.

